Finding bright red blood when you use the toilet, or perhaps feeling a sudden sharp sensation in that sensitive area, can be quite startling, can't it? It's a moment that makes many of us pause, wondering what on earth is going on down there. When we talk about a "hemorrhoid pierced," it usually means a hemorrhoid that has started to bleed, or perhaps even ruptured, which is a rather common, yet often alarming, experience for a lot of people. This isn't just about a little discomfort; it's about seeing something that definitely wasn't there before, like blood, and trying to figure out what it means for your body, you know?
It's very natural to feel a bit worried when you notice blood, especially when it's related to bowel movements. This can be painless bleeding, where you just see small amounts of bright red blood on your toilet tissue or in the toilet bowl itself. Sometimes, too, it's almost a sense of pressure or discomfort that brings it to your attention, rather than just the sight of blood. Understanding what's happening can help ease some of that worry, and that's what we're here for today, to give you some clear information.
In 2024, many people experience issues with hemorrhoids, which are essentially swollen veins in your lower rectum and around your anus, very similar to varicose veins you might see in legs. When one of these veins becomes fragile or is put under strain, it can bleed, which is often what people mean when they say a hemorrhoid feels "pierced" or has "burst." We'll explore what this sensation means, what steps you can take at home, and perhaps most importantly, when it's a good idea to chat with a health care provider about what's going on.
Table of Contents
- What Are Hemorrhoids, Anyway?
- When a Hemorrhoid Seems "Pierced": What It Means
- Taking Care at Home When a Hemorrhoid Bleeds
- When to Seek Professional Help
- Frequently Asked Questions (FAQs)
What Are Hemorrhoids, Anyway?
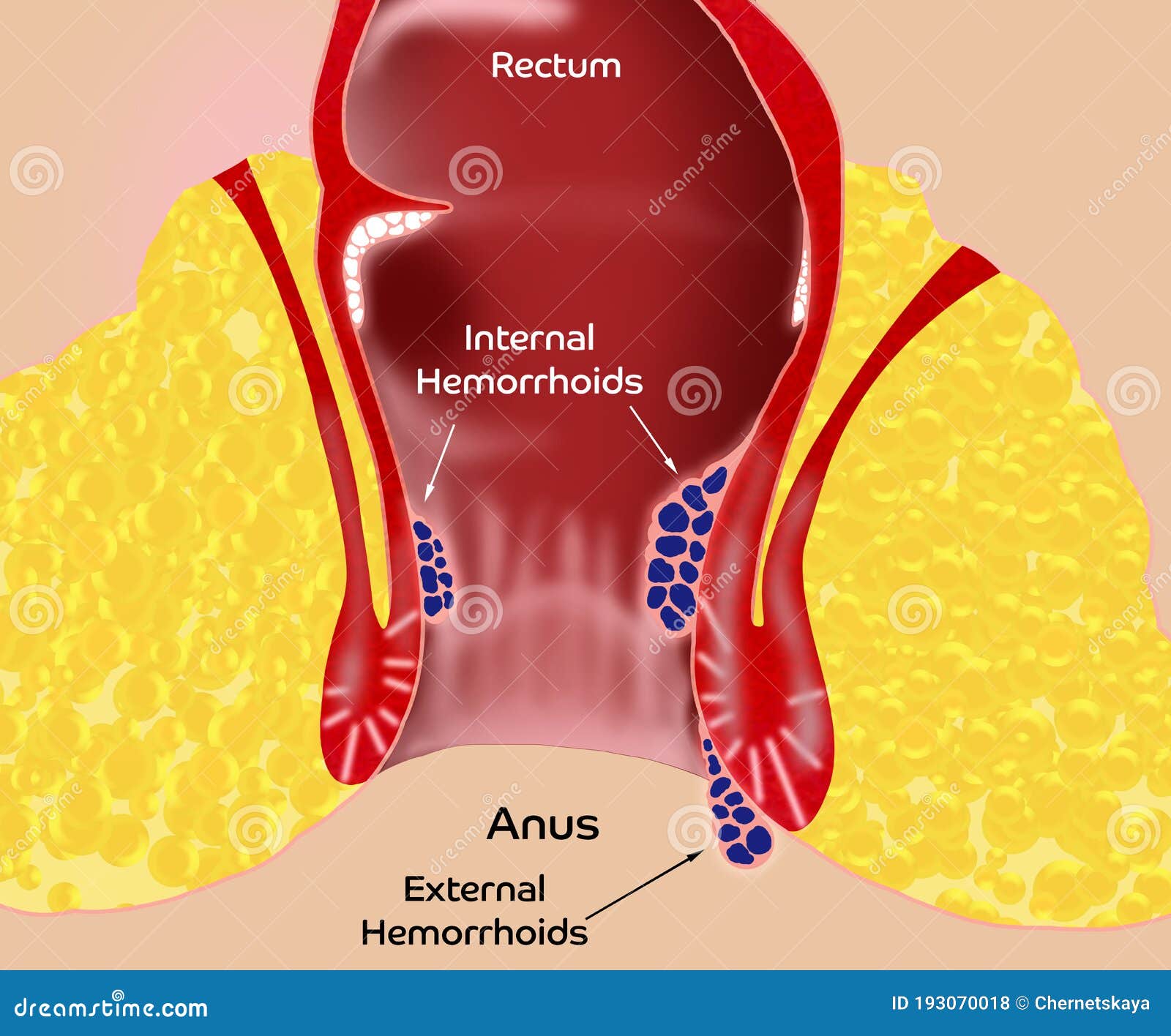
Hemorrhoids, which some people call "almorranas," are swollen veins. They are located in your lower rectum and around the opening of your anus. Think of them, in a way, like varicose veins, but in a rather different spot. These veins can swell up due to various pressures, and depending on where they are, they get different names and cause different feelings. Internal hemorrhoids are inside the rectum, and external ones are outside, around the anal opening.
It's interesting, actually, that internal hemorrhoids are normally painless, but they do tend to bleed. You might not even feel them at all, just see the blood. External hemorrhoids, on the other hand, may cause pain. This distinction is quite important because it often guides how they are treated, or so it seems. So, when you're experiencing symptoms, knowing which type you might have can really help understand what's going on.
When a Hemorrhoid Seems "Pierced": What It Means
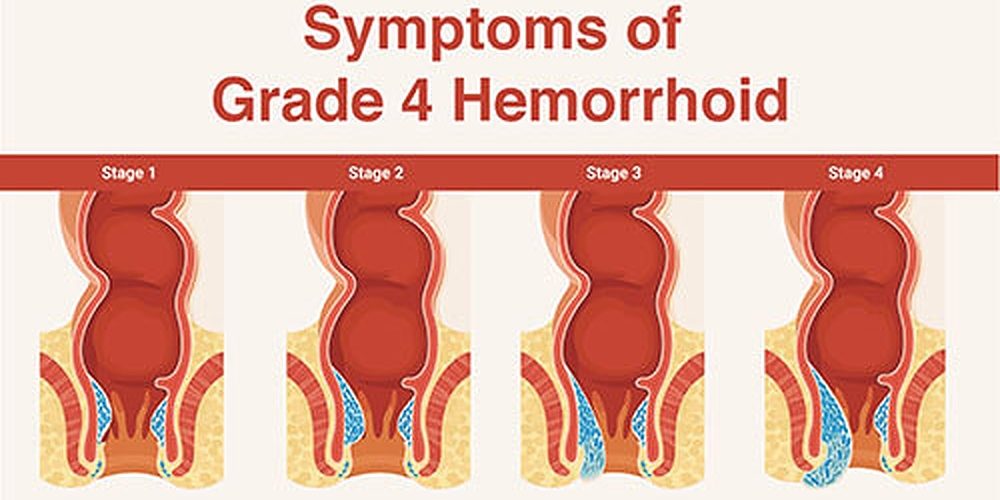
When someone talks about a "hemorrhoid pierced," they are usually describing a situation where a hemorrhoid has ruptured or is actively bleeding. It’s not necessarily like a needle has gone through it, but more that the delicate wall of the swollen vein has given way. This can happen pretty suddenly, and it often leads to visible blood. This sensation or sight can be quite alarming, making people wonder if something serious is happening, which is a very normal reaction, you know?
The Signs of a Bleeding Hemorrhoid
The most obvious sign of a hemorrhoid that has "pierced" or ruptured is bleeding. This often appears as painless bleeding during bowel movements. You might notice small amounts of bright red blood. This blood could be on your toilet tissue, or you might see it in the toilet bowl itself. It's usually a clear, fresh red color, which is a key detail, really.
Besides the blood, there can be other sensations. Patients may also have itching, sometimes called pruritus, around the anal area. You might feel a sense of pressure or discomfort, or even like you haven't completely emptied your bowels. There can also be rectal seepage, which is just a little bit of fluid or mucus that leaks out. For external hemorrhoids, there might be pain, too, which is different from the typically painless internal ones, as a matter of fact.
Why Do Hemorrhoids Bleed or Rupture?
Hemorrhoids bleed because the veins become swollen and thin-walled, making them quite fragile. When there's pressure or strain, like during a bowel movement, these delicate walls can tear or rupture. This is particularly true if you are straining a lot, or if the stool is hard. Sometimes, a hemorrhoid might even push through the anal opening, which can make it more vulnerable to injury and bleeding, naturally.
The pressure from straining, or even just sitting for long periods, can cause these veins to become engorged and more prone to bursting. It's a bit like an overfilled balloon; too much pressure, and it might just pop. This is why managing bowel habits and reducing strain is often a big part of dealing with hemorrhoid issues, you see.
Taking Care at Home When a Hemorrhoid Bleeds
When a hemorrhoid starts to bleed, your first thought might be panic, but there are several things you can do right away to help yourself feel better and encourage healing. These steps are usually pretty simple and can make a big difference in managing the discomfort and promoting recovery, or so it seems. Many times, with these treatments, hemorrhoid symptoms often go away within about a week.
Soothing the Area and Reducing Swelling
One of the most comforting things you can do is soak the area in warm water. Soaking in a warm bath or using a sitz bath with plain water for 10 to 15 minutes, two or three times a day, may really help reduce hemorrhoid swelling. The warmth can be very soothing, and it helps relax the muscles around the anus, which can lessen pressure and discomfort, too. This is a very common and effective home remedy.
For some quick relief from swelling and discomfort, ice packs or cold compresses also can ease symptoms. You can gently apply a cold pack wrapped in a cloth to the affected area for a short period. This can help constrict the blood vessels and reduce inflammation. Just remember not to apply ice directly to the skin, as that could cause more harm than good, you know?
Daily Habits for Relief and Healing
Beyond immediate soothing, making some changes to your daily routine can help prevent further bleeding and promote healing. One important aspect is managing your bowel movements. Eating foods with plenty of fiber and drinking enough water can help keep your stools soft and easy to pass. This reduces the need to strain, which is a major factor in hemorrhoid flare-ups and bleeding, as a matter of fact.
Also, try to avoid sitting on the toilet for too long, and don't strain during bowel movements. If you feel the urge to go, try to go. Holding it in can make stools harder and worsen the problem. Gentle cleaning after using the toilet, perhaps with moist wipes instead of dry paper, can also prevent irritation to an already sensitive area. These small changes can really add up to a lot of comfort and help in the healing process, you see.
When to Seek Professional Help
While many hemorrhoid symptoms often go away on their own or with home care within a week, there are times when it's really important to talk to a health care provider. It's better to be safe than sorry, especially when blood is involved. Knowing when to reach out can prevent bigger problems and get you the right kind of support, you know?
Important Signs to Watch For
You should definitely see your health care provider within a week if you don't get relief from home treatments. If the bleeding continues, or if it becomes heavier, that's a sign to get professional advice. Contact your provider sooner if you experience significant pain, or if the bleeding is constant or seems to be getting worse. Any new or worsening symptoms, like a lot of discomfort, persistent pressure, or increased rectal seepage, should prompt a call, too.
It's also very important to consider if something else could be causing the pain or bleeding. While hemorrhoids are a common reason, other conditions can cause similar symptoms, and a provider can help figure that out. They can rule out more serious issues, which is why it's always a good idea to get a proper check-up if you're concerned. You can learn more about digestive health from reliable sources like the National Institute of Diabetes and Digestive and Kidney Diseases.
What a Health Care Provider Might Suggest
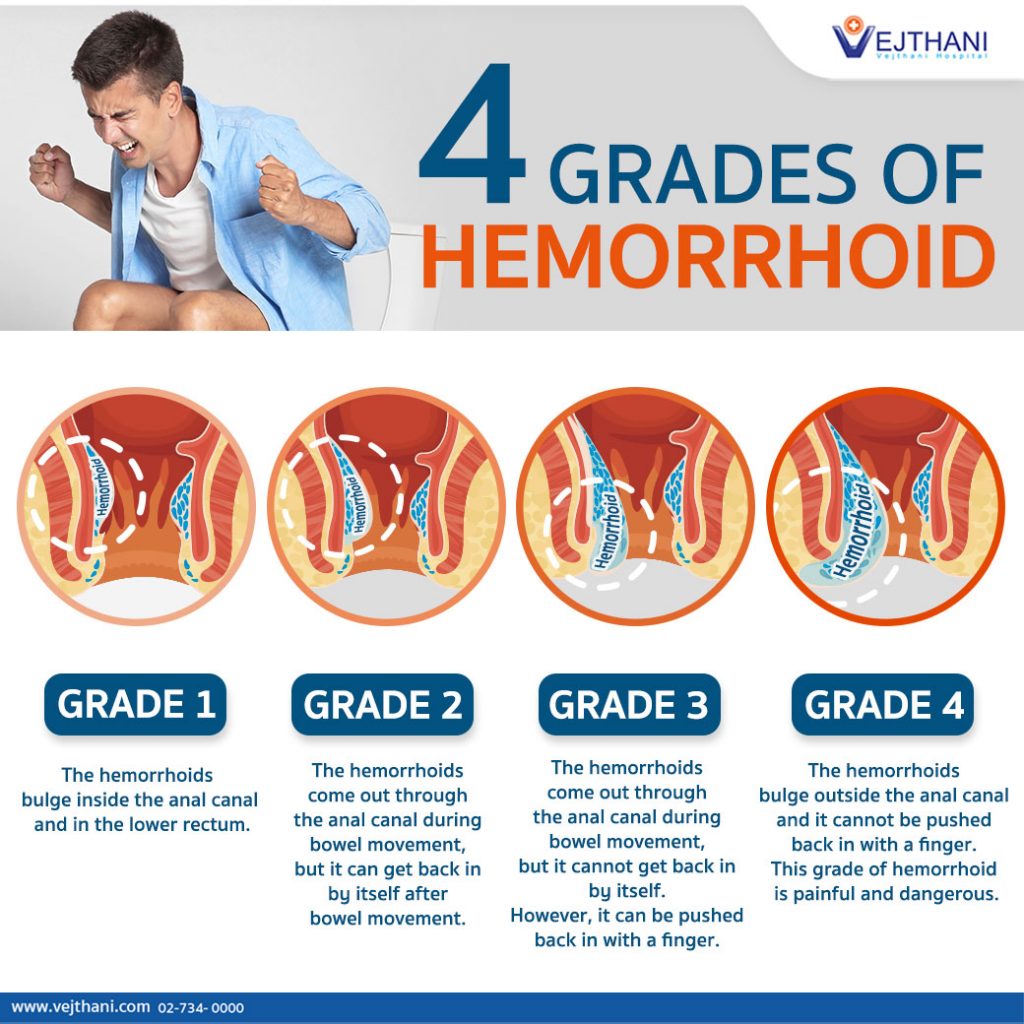
When you see a health care provider for hemorrhoids, they will assess your situation. For internal hemorrhoids, which are often the ones that bleed painlessly, they might suggest specific treatments. For example, to remove a hemorrhoid, they might use a procedure called rubber band ligation. In this method, a health care provider inserts a small tool called a ligator through a lighted tube, which is called a scope, into the anal canal. They then gently grasp the hemorrhoid and place a tiny rubber band around its base. This cuts off the blood supply, and the hemorrhoid eventually shrinks and falls off, usually in a few days. This is a common and quite effective procedure, apparently.
It's worth noting that when we’re talking about hemorrhoid therapy and interventions for hemorrhoids that we can do in a GI setting, we’re only really talking about internal hemorrhoids. We cannot put in rubber bands for external hemorrhoids, for instance, as they are treated differently. Mayo Clinic surgeons are highly experienced in treating hemorrhoids, including the most complicated cases, so you can generally feel confident seeking their expertise for these kinds of issues. They can help you figure out the best path forward for your specific situation. Learn more about hemorrhoid care on our site, and also find information on managing discomfort.
Frequently Asked Questions (FAQs)
What happens if a hemorrhoid bursts?
If a hemorrhoid bursts, it usually means it has started to bleed. This often appears as bright red blood on toilet paper or in the toilet bowl. While it can be alarming, it's generally not an emergency unless the bleeding is heavy or persistent, or if you feel very unwell. You might experience some relief from pressure after it bleeds, actually.
Is a bleeding hemorrhoid serious?
Most of the time, a bleeding hemorrhoid is not serious and can be managed with home care. However, any bleeding from the rectum should be checked by a health care provider to make sure it's actually a hemorrhoid and not something else. If the bleeding is heavy, continuous, or accompanied by dizziness or weakness, you should seek medical attention very quickly.
How do you treat a ruptured hemorrhoid at home?
For a ruptured or bleeding hemorrhoid at home, you can try soaking in a warm sitz bath for 10 to 15 minutes, two or three times a day, to help reduce swelling and discomfort. Applying ice packs or cold compresses can also ease the symptoms. Keeping your stools soft by eating fiber and drinking water, and avoiding straining during bowel movements, are also very helpful steps to take.
Detail Author:
- Name : Dr. Haylee Price
- Username : christiana99
- Email : kari45@gmail.com
- Birthdate : 1977-05-16
- Address : 66753 Roberts Inlet Apt. 989 East Vincenza, MS 10876-2204
- Phone : 475-314-0346
- Company : Crona Ltd
- Job : Photographic Developer
- Bio : Id in occaecati soluta eaque quasi ex. Voluptatem omnis aut doloribus odio non exercitationem facilis sint. Est dolore aut quibusdam exercitationem inventore error tempore.
Socials
facebook:
- url : https://facebook.com/jakeroberts
- username : jakeroberts
- bio : Dolorem quaerat quia ut voluptatem expedita soluta aut.
- followers : 4745
- following : 2905
linkedin:
- url : https://linkedin.com/in/jake_roberts
- username : jake_roberts
- bio : Est sint quo aut.
- followers : 4568
- following : 1134

